The term pancreatitis defines an inflammatory process that is localized in the tissues of the pancreas (pancreas). Acute or chronic course of the disease of varying severity leads to a violation of the functional state of the organ, which affects the digestion process. Treatment of pancreatitis, regardless of the severity of the course, the nature and origin of the pathological process, necessarily includes the use of dietary recommendations. According to the classification of diets, the table for pancreatitis is marked with 5p.
The main feature of the diet
The main goal of the diet in acute or chronic pancreatitis is a significant decrease in the functional load on the pancreas, which contributes to the rapid decrease in the severity of the inflammatory process. The diet has some of the following distinctive features:
- The diet reduces the amount of carbohydrates (mainly due to sugar and other easily digestible disaccharides) and fats.
- Increase the protein content in the diet.
- A sharp restriction in the intake of extractive organic compounds, purine bases, refractory fats, essential oils, cholesterol, coarse fibers, which significantly increase the load on the organs of the digestive system.
- Increase the content of lipotropic compounds and vitamins.
- Dishes must be steamed or boiled. Food stew is limited. Avoid fried foods.
- The number of cold and too hot dishes is limited.
The chemical composition, the daily content of the main organic compounds and the energy value of the diet for pancreatitis include the following indicators:
- Proteins - 110-120 g, of which 60-65% should be of animal origin.
- Carbohydrates - 350-400 g, of which 30-40 g of sugar are allowed. It is recommended to take 20-30 g of xylitol sweetener.
- Fats - 80 g, of which 15-20% of plant origin.
- Table salt (sodium chloride) - 10 g.
- Free liquid - 1. 5 liters.
- Energy value - 2600-2700 kcal.
The recommended food intake is 5-6 times a day, while single portions should be small. This allows to reduce the load on the entire digestive system in general and on the pancreas in particular.
Mechanism of therapeutic action
The pancreas is a functionally important organ of the digestive system. It produces numerous digestive enzymes (proteases, lipases, amylases) which are responsible for the breakdown of proteins, fats and carbohydrates in the lumen of the small intestine. With the development of an inflammatory reaction provoked by various reasons, damage to the glandular cells and tissue edema occur. At the same time, compression of the excretory ducts of the pancreas develops, the outflow of the contents is disturbed, which can subsequently lead to tissue death, provoked by the release of digestive enzymes (pancreonencosis). To prevent the complications of inflammation, it is important to reduce the load on the pancreas, for which the 5p diet was developed.
The essence of dietary recommendations is to significantly reduce the amount of carbohydrates and fats that accompany food. This at the regulatory level causes a decrease in the functional activity of the pancreas, the production of digestive enzymes and the likelihood of developing pancreatic necrosis decrease. Frequent meals divided into small portions allow to reduce the load on all organs of the digestive system, which helps to quickly reduce the severity of the inflammatory process in the pancreas. By increasing the amount of lipotropic compounds and vitamins, it is possible to improve the course of metabolic processes in the tissues of the liver and other parenchymal organs of the digestive system.
Indications
The implementation of dietary recommendations is indicated in the development of chronic pancreatitis in remission (improvement of functional status) or in the acute course of the inflammatory process during the period of convalescence (recovery). Also, the diet can be used for combined inflammation of the pancreas, gallbladder, liver.
Contraindications
With a pronounced acute course of the inflammatory process, the use of a diet for pancreatitis is not recommended, since in this case table 0 (complete lack of nutrition) is prescribed for a period of up to several days. The main nutritional organic compounds in the form of monomers are administered parenterally by intravenous drip (amino acids, glucose). Also, if necessary, intensive treatment is prescribed using drugs of various pharmacological groups.
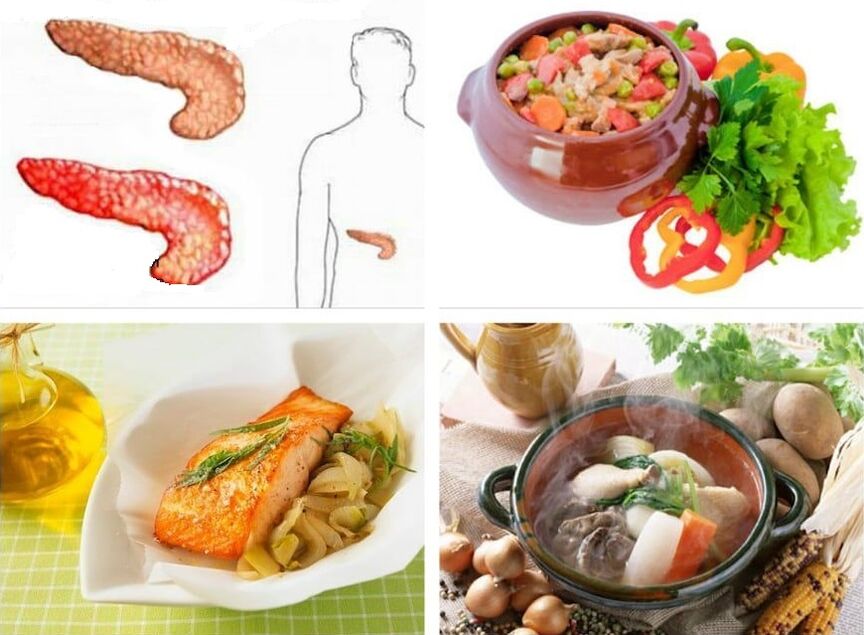
Permitted products
The use of a diet for pancreatitis involves the intake of permitted foods, the list of which is quite diverse and includes:
- The first courses are soups boiled in water with the addition of vegetables (carrots, potatoes, pumpkin, zucchini), cereals (semolina, rice, buckwheat), vermicelli, a small amount of butter is allowed.
- Meat - lean meats, which include chicken, rabbit, veal, beef, skinless turkey. Before cooking, the meat is freed from the skin (poultry), tendons. It is recommended to boil it or steam it.
- Vegetables - potatoes, cauliflower, zucchini, peas, carrots, beets, boiled, baked or steamed pumpkin.
- Cereals - cereals from oats, buckwheat, semolina, rice, which are cooked in water or with a little milk. They can also be added to soufflés and puddings.
- Ripe, sweet fruits or berries that can be eaten fresh or baked.
- Dairy products - low-fat whole milk in limited quantities, subject to its normal tolerance, yogurt, cottage cheese, cream.
- Desserts: mousse, jelly, jelly, jam, which are prepared with xylitol (a sweetener).
- Chicken eggs - limited, 2 pieces per day in the form of omelettes.
- Flour products - yesterday's bread made from wheat or rye flour, lean products.
- Fats - butter, vegetable oil.
- Drinks: green and weak black tea, fruit juices, compotes, rosehip broth.
Prohibited products
Against the background of the implementation of dietary recommendations for pancreatitis, the use of the following foods is excluded:
- Soups, cabbage soup, borsch on meat, fish broth, beetroot, okroshka.
- Fatty meats (duck, goose, pork, lamb), fried, stewed dishes from it, smoked meats, sausages.
- Fatty fish, fried, stewed, salted, caviar, canned.
- All dairy products rich in fat and sugar, including lactose (milk sugar).
- Legumes, the use of barley, corn, pearl barley and crumbly cereals is limited.
- White cabbage, turnip, sorrel, sweet pepper, eggplant, radish, onion, garlic, spinach, mushrooms, radish.
- Spices, spicy, fatty sauces, especially those cooked in meat broth.
- Coffee, cocoa, carbonated and cold drinks.
- Pastry cream, chocolate, ice cream, sweets containing a considerable amount of sugar.
- Animal fats.
Nutritional characteristics
Proper use of the pancreatitis diet involves adhering to some of the following nutritional recommendations and habits:
- The menu for acute pancreatitis or exacerbation of a chronic process includes a mandatory saving regime. The amount of food is severely limited up to temporary curative hunger (diet 0). When the severity of the inflammatory process subsides, the menu gradually expands, but the food is served in a flattened form.
- In chronic pancreatitis, a 5p diet is used without a sparing regimen. It includes the usual temperature regime with the obligatory exception of very hot and very cold dishes.
- The acute course of the inflammatory process in the tissues of the pancreas requires the hospitalization of a person in a medical hospital, where the doctor determines the dietary recommendations. If there is a high probability of developing pancreatic necrosis in the first days, a 0 diet is prescribed under strict medical supervision.
- It is recommended to take food at least 5 times a day in small portions, which allows you to significantly reduce the load on the pancreas.
- It is recommended to have the last meal no later than 2 hours before the expected sleep. In modern recommendations, the time period between dinner and bedtime has increased to 3-4 hours.
- In chronic pancreatitis, a diet is prescribed for a long time, which is necessary mainly to prevent an exacerbation of the inflammatory process in the tissues of the pancreas.
Sample menu for the week
Monday
- Breakfast: buckwheat porridge boiled in milk, bread and butter, weak black tea.
- Lunch - fresh pear.
- Lunch - vegetable soup, boiled in water, noodle casserole with chicken, apple jelly.
- Snack: biscuits, rosehip broth.
- Dinner: boiled fish without bones, mashed potatoes with a small amount of butter, green tea.
Tuesday
- Breakfast - boiled vegetable vinaigrette, cheese sandwich, green tea.
- Lunch - cottage cheese casserole with the addition of plums.
- Lunch: milk soup with rice, stewed carrots with boiled chicken, fruit compote.
- Afternoon snack - lean cookies with freshly squeezed fruit juice.
- Dinner - pasta with cottage cheese, boiled in water, jelly.
Wednesday
- Breakfast: apple and carrot salad, chopped steamed cutlets, fruit juice.
- Lunch is a baked pear.
- Lunch - vegetable soup boiled in milk, boiled boneless fish with rice porridge, fresh fruit.
- Snack - biscuit biscuit, compote of dried fruit.
- Dinner: rice porridge cooked in milk, cheese sandwich, apple compote.
Thursday
- Breakfast - semolina porridge, boiled in milk, with the addition of plums, weak black tea.
- Lunch - carrot puree with apple jam.
- Lunch: vegetable soup cooked on a decoction of dried fruit, cottage cheese pudding, baked apple.
- Snack - fruit jelly.
- Dinner: Buckwheat porridge, boiled in water, with steamed beef cutlets, natural mineral water.
Friday
- Breakfast - cheesecake with carrots, black tea.
- Lunch: cottage cheese with low-fat sour cream.
- Lunch - soup with barley and carrots, boiled in water, cabbage rolls cooked with rice and boiled chicken meat, fruit jelly.
- Snack - sweet fresh apple.
- Dinner: potatoes boiled in water, boiled fish without bones, kefir, a piece of bread.
Saturday
- Breakfast - cheesecake with fruit jam, green tea.
- Lunch is a fresh banana.
- Lunch - borscht cooked in vegetable broth, casserole made from vegetables and chicken, fruit compote.
- Snack - dry biscuit, composed of dried fruit.
- Dinner - casserole with pasta and boiled beef, kefir.
Sunday
- Breakfast - soup with potato dumplings, boiled in milk, weak black tea.
- Lunch is a fresh sweet apple.
- Lunch - cabbage soup cooked in vegetable broth, boiled pasta with steamed cutlets, compote.
- Snack: biscuits, rosehip broth.
- Dinner: an omelette made from chicken eggs, lazy dumplings with cottage cheese, kefir.
Opinion of the doctor
The pancreatitis diet is biologically healthy. By reducing the functional load on the pancreas, the risk of complications, including pancreatic necrosis, is significantly reduced, and the inflammatory process in the tissues of the organ is also accelerated. At the same time, the severity of edema decreases, the outflow of pancreatic juice and bile improves, which contributes to the normalization of the functional activity of all organs of the digestive system. Dietary recommendations are aimed at reducing the functional load on the pancreas during the period of attenuation of acute inflammation or against the background of the chronic course of the disease. In the case of acute pancreatitis, due to the high risk of developing pancreatic necrosis in a medical hospital, diet 0, which is therapeutic starvation, can be prescribed.














































































